
2023 · September
AI biomarkers to transform oncology

Alan Aberdeen
Co-founder
AI biomarkers will transform oncology with new maps for tumor biology and breakthrough predictors for treatment response. We have the opportunity to improve outcomes for every cancer patient with AI-driven insights from digital pathology.
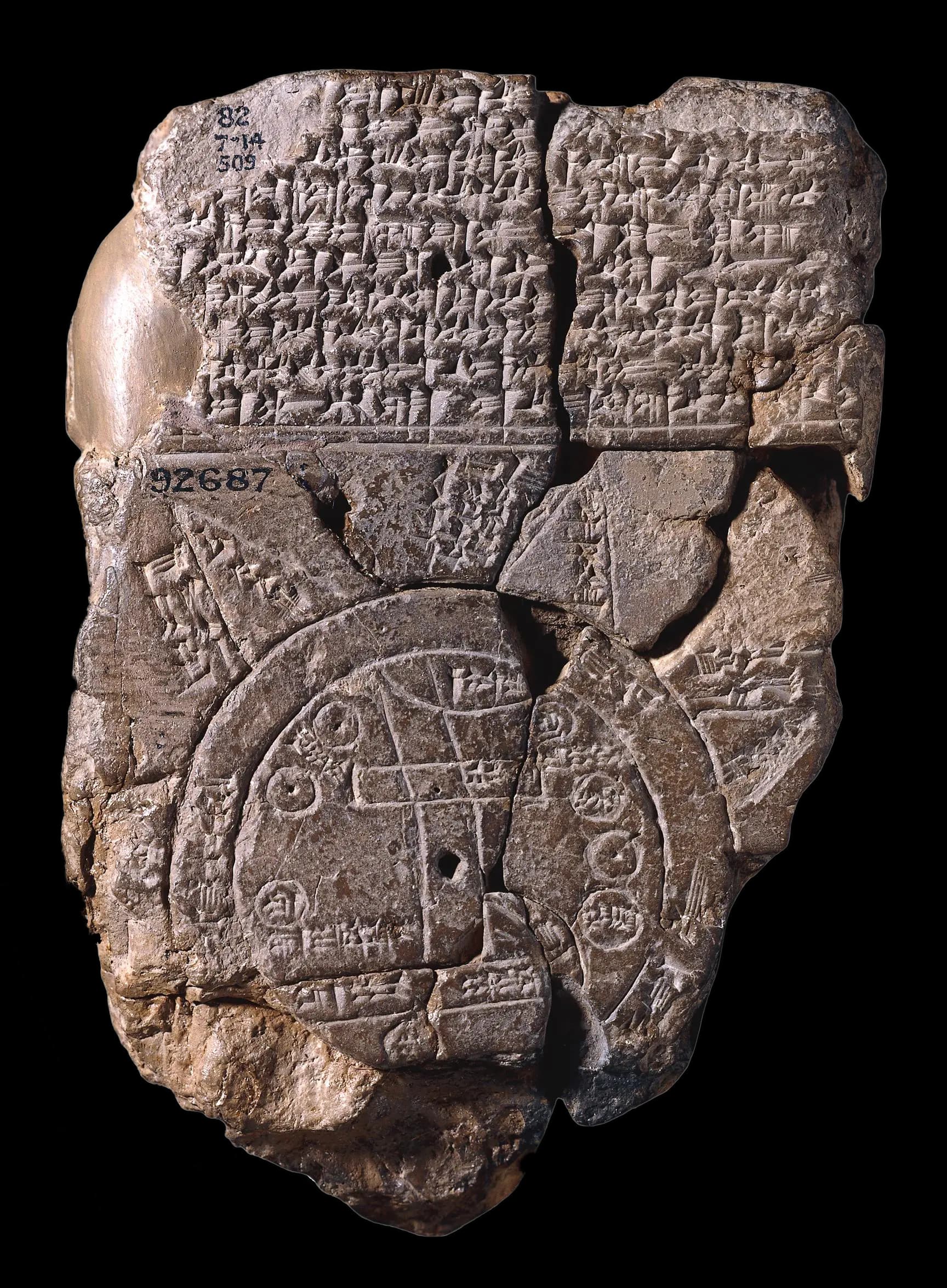
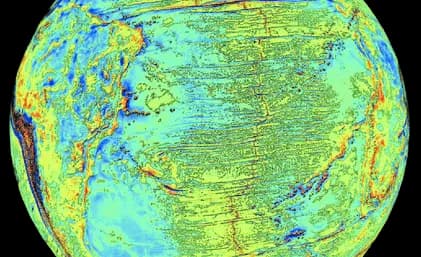
I love maps. They are wonderful tools and one of our greatest achievements, enabling us to explain and navigate our way through the world. Maps inform our knowledge of the world; their quality reflects the level of our scientific understanding - from the earliest classical flat earth depictions to modern three-dimensional topography of the ocean floor.
Robert Hook, a mapmaker himself, refined the design of the compound microscope, and was one of the first to start to map the biological world with large-scale, finely detailed illustrations.
This micro-scale view is essential for understanding disease. In cancer particularly, the tumour microenvironment is a busy place. Cancer cells grow and divide very rapidly, interacting with various cell types and changing the environment around them. Histopathologists lean on their clinical experience, knowledge of cancer biology, and critical thinking to accurately interpret and analyse a plethora of these cellular interactions. They identify the critical "landmarks" on the map that can provide insights to better diagnose patients and guide treatment decisions.
Today, initiatives like the Human Cell Atlas are making strides in creating reference maps for all human cells. They use technological advancements which allow us to classify cells by their RNA expression profiles, digitally image tissue, and catalogue cells based on shape, location, and function.
Validating tumour tissue "landmarks" or "biomarkers" is a daunting task. At best, clinical histopathologists can give the gestalt impression from what they see, a reflection on their experience and similar cases they've seen before. Frequently, this leads to pathologists disagreeing with each other. A recent study in colorectal cancer found interobserver discrepancy in 53% of cases. To address this, the pathology community has developed guidelines to standardise reporting. By necessity these are often categorical and coarse - asking the human expert to compress the signal in hundreds of thousands of cells to a single number. This isn't to say they have no value, all models are wrong, but some are useful.
But we can do better. What we need, and what we have the opportunity to build today, is both better maps of tumour biology through digital pathology and better models through which to find the clinically meaningful "landmarks".
The temptation with a new digital technology is to replicate our analogue methods. An often cited example is how the early web simply mimicked newspapers, putting advertisements next to content and making the web awful.
We need to build new biomarkers, to not just count cells or digitise analogue grading systems. With AI and deep learning, we have the opportunity to build novel tools, new lenses through which to analyse, interpret and better understand the tumour microenvironment.
These tools have the potential to augment the capabilities of histopathologists and clinical teams and move us to a new level of disease understanding. At GTL, our AI biomarkers first map the tissue, and then go beyond that to predict patient survival, expose genetic properties of tumours, and indicate the potential treatment response to a particular drug directly from routine pathology slides.
These novel methods can extract more quantitative information from pathology slides than human experts - they don't simply mimic the analog grading systems of before, they create new insight and knowledge.
This is the new world of computational histopathology and AI biomarkers the killer app. In 2023 we raised a $4.3M seed round on our path to build this future. Join us on our mission to improve outcomes for every cancer patient with AI-driven insights from digital pathology.